Our Green Plan 2025-2028
Our vision for the next decade
At Frimley Health, we are starting an exciting new journey.
Our goal is simple but powerful: to give every person in our community, from newborn babies to older adults, the right care, in the right place, at the right time.
We want to help everyone live healthier and more independent lives.
This strategy is our promise to adapt, improve, and work together, always guided by compassion and effectiveness.
Our clinical strategy is built on four main ideas, which also support the trust’s FHFT 2030 organisational strategy:
- Firm foundations: We use our strengths and always aim for the highest quality and safety. We keep improving, so patients and staff can trust us.
- Care without walls: We bring care out of the hospital and into homes and communities, making it more personal and easier to access.
- Centre of excellence: We want to be the best in both specialist and general care, always aiming for best outcomes for our patients.
- Adding value: We use our resources wisely and make the most of new technology, so every action makes a difference.
The big changes ahead
Healthcare is changing fast. Our community is growing and getting older, with more people living with long-term health needs. We are responding by focusing on three big changes:
- From hospital to community: More care will happen closer to home, so people can stay independent and avoid unnecessary hospital stays.
- From treatment to prevention: We will help people stay healthy, spot problems early, and support self-care.
- From analogue to digital: Technology and data will help both patients and staff, making care safer, faster, and more connected.
Our clinical priorities are the heart of our strategy
We always put patients first. Every service must meet the highest standards for safety and quality.
Our targets include:
- Achieve and maintain a Care Quality Commission (CQC) rating of “Good” or “Outstanding” across all sites and services.
- Meet or exceed the NHS 4-hour Emergency Department standard (95% of patients seen within 4 hours).
- Achieve >95% compliance with infection prevention standard
We want more people to recover at home, with support from virtual wards and community teams. Neighbourhood health hubs and digital tools will help make this happen.
Our targets include:
- Increase the number of patients supported by virtual wards by 30% over the next three years.
- Reduce avoidable hospital admissions by 10% by 2030.
- Ensure 80% of end-of-life care is delivered in the patient’s preferred place.
We are using tools like artificial intelligence and online patient records to improve care. Technology should make things easier, not harder, for patients and staff.
Our targets include increasing the use of digital technology and AI to ensure:
- 100% of patients to have access to their digital health record by 2027.
- 90% of outpatient appointments to be bookable online by 2028.
- Implement at least two new AI-supported clinical pathways per year.
We support people to stay well. By focusing on prevention, screening, and early help, we can stop health problems before they start.
Our targets include:
- Increase uptake of NHS screening programmes (e.g., cancer, diabetes) by 15% in priority groups.
- Reduce smoking prevalence in the local population by 5% by 2030.
- Achieve childhood immunisation rates above 95%.
Everyone should get good care, no matter where they live or their background. We will make our services accessible and sensitive to all cultures and needs.
As part of our commitment to accessible and culturally sensitive services, we will:
- Halve the gap in life expectancy between the most and least deprived communities by 2035.
- All patient-facing materials available in the top five community languages by 2026.
- 100% of staff to complete health inequalities training by 2027.
Our staff are our greatest strength. We will invest in training, wellbeing, and new opportunities, so Frimley Health is the best place to work.
Our targets include:
- Staff vacancy rate below 8% by 2028.
- 90% of staff to complete annual training and development plans.
- Achieve staff survey engagement scores above the national NHS average.
We are expanding planned and specialist care, reducing waiting times, and improving results. Our new hospital and elective hubs will set new standards for patient experience.
Our targets include:
- 92% of patients to receive planned care within 18 weeks of referral.
- Elective surgery cancellation rate below 1%.
- Achieve national cancer waiting time standards (e.g., 62-day referral to treatment).
We want care to be smooth and connected. By joining up hospital, community, and primary care, patient journeys will be easier and more coordinated.
To deliver this we will ensure:
- 100% of discharge summaries are sent to GPs within 24 hours.
- Delayed transfers of care are reduced by 20% by 2030.
- Three new integrated care pathways are launched each year.
We are building a new Frimley Park Hospital, using sustainable designs and the latest technology to make sure our facilities are ready for the future.
Our targets include:
- Start building the new Frimley Park Hospital by 2030.
- Reduce carbon emissions from Trust buildings by 50% by 2030.
- Achieve 100% compliance with NHS digital infrastructure standards.
We encourage research, learning, and innovation, so we keep getting better every day. As part of this commitment, we will:
- Ensure all clinical teams participate in at least one quality improvement project each year.
- Increase patient participation in research studies by 25% by 2030.
- Achieve top quartile performance in national patient experience surveys.
Our community is diverse. We care for:
- Older adults with complex needs
- Working-age adults focused on prevention and mental health
- Children and young people needing early support
- Ethnic minorities needing accessible and sensitive services
- People with disabilities or long-term conditions who need tailored support
Bringing the strategy to life
In every area, urgent and emergency care, planned care, women’s health, children’s services, cancer, ageing well, and more, our approach is joined by one thread: compassion and quality in every moment.
We are investing in virtual hospitals, community diagnostic centres, better digital access, and new buildings. Our focus on prevention, early help, and joined-up care will help people stay well and live independently for longer.
What this means for you
- Patients will have easier access, more choices, and care that fits your life.
- Staff will get support, training, and the chance to innovate and improve.
- Communities will see a healthier, more independent population, with fairer services designed around your needs.
Our commitment
This is more than just a plan, it is a story of transformation.
By working together, using new ideas, and staying true to our values, we will deliver compassionate, effective, and modern healthcare for everyone in our community, now and for the future.
Our clinical strategy in full
Introduction
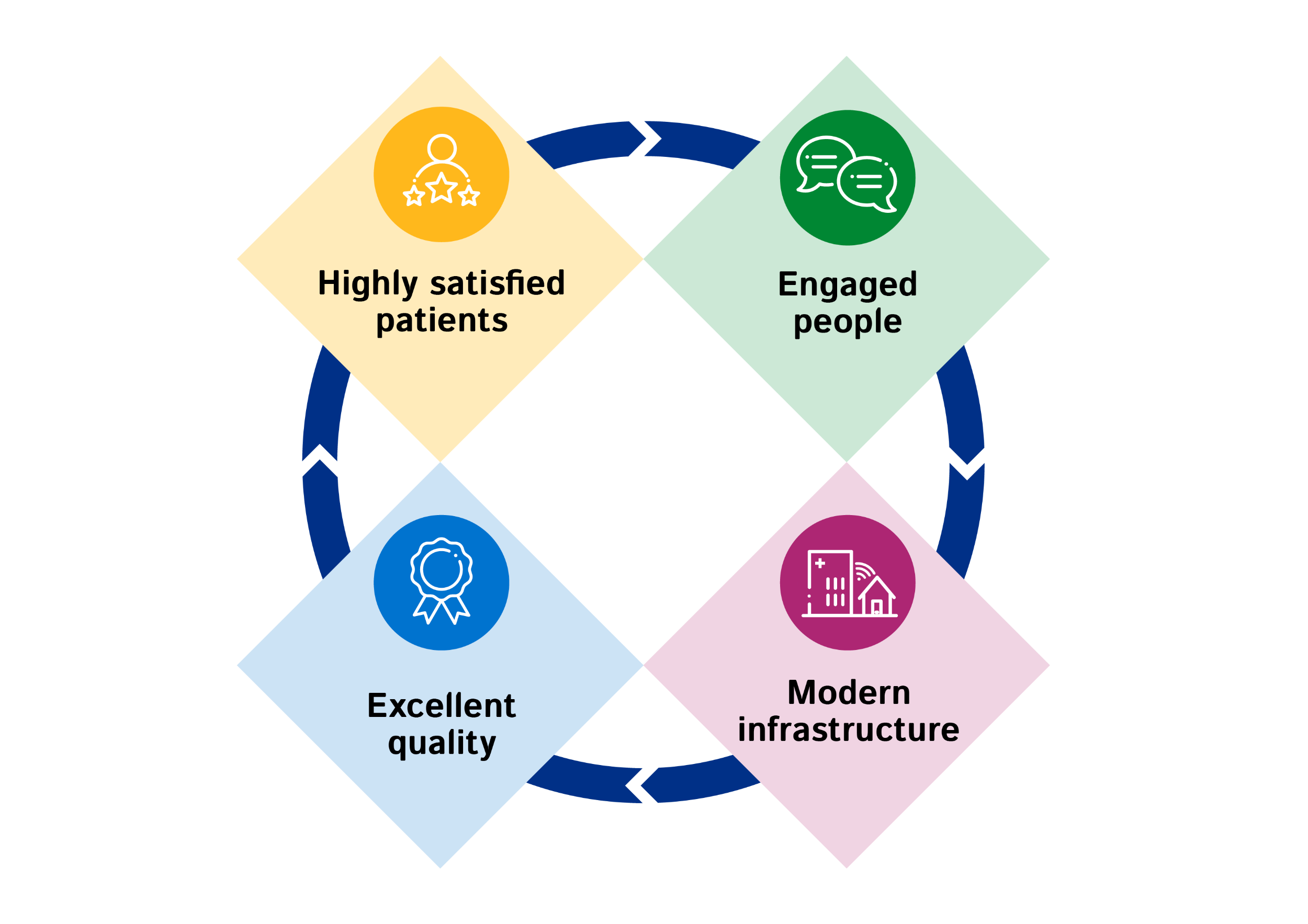
Frimley Health’s ambitious clinical strategy sets the direction for our clinical services to achieve our Trust vision to be compassionate, effective and modern in all that we do for a population whose health needs and expectations will change over the next 10 years. We will achieve this by focusing on our patients, people,
quality and infrastructure and through our behaviours that are guided by our three values.
In developing this strategy, four guiding principles have been developed that underpin our clinical service ethos: firm foundations, a centre of excellence, care without walls, and adding value.
Our clinical strategy 2035 outlines our vision to deliver clinical services over the next 10 years, addressing the current and future healthcare needs of our local population. We worked closely with our clinical teams and system partners to develop our clinical strategy, drawing on Lord Darzi’s recommendations and the emerging 10-year plan.
Our journey to developing the clinical strategy 2035 commenced in November 2023, with a series of workshops to understand the current and future state, from which draft clinical principles were developed and refined.
Further workshops took place during 2024 to align our direction to the evolving national strategy, guidance and NHP requirements, and the Trust strategy.
Clinical theme workshops were held in November 2024 and further feedback and engagement sessions have taken place to produce this strategy.
Our clinical strategy sets out our vision to address our current and future challenges, which are:
- Increasing demand for health and social care services across our system.
- An aging population, with more having two or more medical conditions.
- Patients waiting longer for care than they should.
- Challenges accessing services for certain demographics and working-age people.
- Health inequalities that exist within our local geography.
Increasing delivery of care closer to home in the community will mean a shift in resources, clinician skills and models of care in order to provide compassionate, effective and modern healthcare with best outcomes.
Working with our system partners, we will reduce health inequalities and increase life expectancy, enabling our patients to live better for longer.
Our future clinical models have been developed through evidence-based modelling using our systemwide shared record.
We will design and deliver our new services, our new Frimley Park Hospital and investments in our other sites using this data-focused approach, making decisions through collaboration with our partners.
Services will be joined up and delivered in the context of right care, in the right place and at the right time.
We will use digital technology and AI to support clinical care and enable more safe, personalised, timely and local provision.
Our clinical strategy 2035 is supported by several connected strategies (Trust, People, Digital and Estates) and their linked plans.
A transformation plan, including a target operating model will underpin this strategy with robust governance to ensure effective delivery to ensure we have addressed those challenges as laid out.
Our clinical strategy builds on our success as a leader in excellence and safety in care, alongside innovation and transformation.
Our clinical strategy 2035 builds on our success as a leader in healthcare. We are recognised for our excellence and safety in delivery of the elective care, virtual hospital, local, specialist services and community services. Our Trust, together with our system partners, have demonstrated our ability to deliver innovation and transformation across our system.
- Community services:
In 2020, we extended our care to provide community services to the south of our
integrated care system and have continued to expand our virtual wards and healthcare at home. - Virtual ward:
We have the widest use of virtual wards in the region and continue to grow this service. - Primary care:
We established a strong clinical interface with partners to drive quality improvement. - Community Diagnostic Centre:
This will be opened in Slough in 2025 for diagnostics and one- stop clinics for key pathways to grow this service. - Heatherwood Hospital:
We became one of the first GIRFT-accredited and re-accredited six-day elective surgical hubs in the NHS. - Our connected care record and dataset:
Integrates health and care information to better understand disease and model future demand. - Our AI working group:
Won the Excellence in Healthcare Award at the NHS Parliamentary Awards and was highly commended at the Health Service Journal digital awards for the AI-assisted cataract ‘Dora’ pathway - Getting It Right First Time (GIRFT):
Adoption of GIRFT around key pathways, reducing waiting times, length of stay and improving patient experience, specifically:- Reduced length of stay joint replacements
- Improvements in theatre utilisation across all sites.
- Excellent patient satisfaction rates for the skin cancer hub and its new one-stop clinics.
- Improved advice and guidance response times.
- Reduced waiting list for ears, nose and throat for both adult and paediatric patient.
- Creating a successful cardiology model in partnership with GPs to give more patients rapid access closer to home.
- Continuing to work with our integrated care system to enhance local community services around pathways.
- Electronic patient record:
Launched a state-of- the-art EPR system, integrating over 200 systems, making us one of the most digitally advanced trusts in the country.
Strategic context
Empowering patients, improving productivity, and investing in multidisciplinary teams are essential for delivering higher quality care.
The NHS is facing significant challenges, including workforce shortages, increased demand, and budget pressures. The Lord Darzi independent investigation of the NHS in England 2024 highlighted the worsening health of the nation, with rising long-term conditions and mental health issues. Patients struggle to see GPs, waiting lists are long, and emergency departments are overwhelmed.
There are over 100,000 vacancies for key posts. Recommendations for the future include shifting care from hospitals to communities, embracing digital solutions, and focusing on prevention. Empowering patients, improving productivity, and investing in multidisciplinary teams are essential for delivering higher quality care.
Frimley Health is the only acute trust within our integrated care system which covers five areas: North East Hampshire and Farnham, Bracknell Forest, Windsor and Maidenhead, Slough and Surrey Heath.
Together with our integrated care system we successfully developed Connected Care which brings together data from across the system, enabling Frimley Health to understand current and future population health and care needs.
Through our detailed analysis, we know that there are health inequalities across our integrated care
system with an increasing age and morbidity trajectory.
Across our system working with NHS Surrey and Borders and NHS Berkshire Healthcare, we developed our joint forward plan. The plan has three overarching objectives:
- To improve the health and wellbeing of our communities.
- To provide high-quality care to all our patients.
- To ensure that our healthcare services are sustainable for the long term.
At the time of writing this strategy, the NHS landscape and local system structures continue to evolve.
Frimley Health
Frimley Health provides care across three hospital sites and community locations and serves a diverse population.
Frimley Health also provides specialist services to other care systems, and we continue to work closely with multiple providers in the region, as the demands on these services evolve.
Our extensive Trust-wide GIRFT further faster programme and Frimley Excellence (continuous quality improvement) provide our teams with knowledge, tools and skills to improve how we work and pathways to improve clinical outcomes. We have many other quality improvement initiatives that underpin our culture where quality and safety are paramount.
Infrastructure challenges include the condition of Wexham Park and Frimley Park hospitals, with redevelopment plans in place.
The new electronic patient record (EPR) system and MyFrimleyHealth Record enhance digital capabilities, with Heatherwood Hospital and the new Community Diagnostic Centre in Slough (opening late 2025) providing high-quality care.
Our local area
Across our local integrated care system we work with local and regional partners to deliver care to our population and beyond. These include health and social care partners, as well as private and third sector organisations.
By working across geographical and organisational boundaries, we aim to deliver a complete service to local people, communities and staff to improve their health and wellbeing, and to use our collective resources more effectively.
These partnerships aim to help ‘create healthier communities with everyone’. Our integrated care system has recently refreshed their five-year strategy ‘Creating Healthier Communities’ which tackles the wider determinants of health and wellbeing for our population. These priorities will remain as future organisational and commissioning models evolve.
Through the Joint Forward Plan, we will:
- Address current and future workforce challenges.
- Maximise sharing of information to reduce gaps in care.
- Improve communication with patients and between services.
- Improve our ability to monitor health and needs remotely.
- Improve our provision for mental health.
- Increase capacity for elective care to six days.
- Increase efficiency around urgent and emergency care services, ensuring patients access the most appropriate service.
Partner Trusts and NHS organisations
- Berkshire Healthcare NHS Foundation Trust
- Frimley Integrated Care Board (ICB)
- Buckinghamshire, Oxfordshire & West Berkshire (BOB) Integrated Care Board (ICB)
- Surrey and Borders Partnership NHS FT
- South-East Coast Ambulance Service NHS FT
- South Central Ambulance Service NHS FT
- Primary care networks (x16)
- HCRG Care Group
Local and voluntary organisations
- Local Healthwatch organisations
- Voluntary sector organisations
Local Council partners:
- Royal Borough of Windsor and Maidenhead
- Surrey County Council
- Hampshire County Council
- Surrey Heath Borough Council
- Rushmoor Borough Council
- Hart District Council
- Waverley Borough Council
- Bracknell Forest Council
- Slough Borough Council
About our population
The impact of population growth, demographics, and epidemiology - particularly the impact of growth in older people with multiple long-term conditions, will determine the shape of demand for health and care services in the future and the service provision at Frimley Health. We need to better integrate with system partners to provide compassionate, effective and modern healthcare.
2025 population c.800,000
2036 population c.847,000
The significant growth in older people is not matched by a similar growth in younger years that will form the potential workforce of the future.
Overall, the population is set to increase 5.35% between 2018 and 2041, with differences in growth rates across our geography. However, the needs of that population will increase significantly. The numbers
of people aged 60+ increases dramatically over the planning horizon to 2041.
We predict that our local population will increase by 6.4% by 2036, with the largest increases in the over 60s and teenage age group.
This has informed our projections in relation to future service provision requirements.
People that live in recognised areas of deprivation will often have poorer outcomes and on average will have a lower healthy life expectancy.
Most of our population don’t live in areas of deprivation. All areas contain pockets of deprivation, but they can be less visible due to nearby affluence.
There are 122 different spoken languages in our population. 98,000 residents in our integrated care system do not have English as their main spoken language, the most common are Urdu, Polish and Punjabi.
Language barriers can impact a persons’ ability to access and navigate health and care services.
There is a strong association for diabetes, COPD, heart failure and many other conditions with deprivation. We also see lower prevalence rates for cancer and atrial fibrillation which could reflect under-diagnosis and problems accessing healthcare.
On average, we see many conditions are between one and a half to two times more prevalent in deprived areas after adjusting for age and sex of the population.
When looking at ethnicity data, we notice the following:
- Asian/Asian British notably higher for diabetes, non-diabetic hyperglycaemia and coronary heart disease, lower for depression, COPD and atrial fibrillation.
- Black/Black British notably higher for diabetes, hypertension, chronic kidney disease and obesity, lower for COPD, depression, and atrial fibrillation.
| percentage from BAME ethnicity groups | percentage living in deprivation | percentage over 65 | percentage in households of more than 5 people | |
|---|---|---|---|---|
| Bracknell Forest | 11% | 4% | 14% | 26% |
| North East Hampshire and Farnham | 11% | 13% | 17% | 28% |
| Royal Borough of Windsor and Maidenhead | 16% | 5% | 17% | 32% |
| Slough | 61% | 61% | 9% | 52% |
| Surrey Heath | 12% | 7% | 18% | 28% |
| Whole population | 23% | 19% | 15% | 34% |
Our guiding clinical principles
Four clinical principles were developed to underpin our clinical strategy.
Firm foundations:
Building on our solid foundations for the future
We will build on our existing strengths and work with system partners to deliver excellent quality, compassionate care that is shaped by population healthcare needs, and provide equitable access and reduce health care inequalities.
- We will maintain our high performance and delivery standards. Quality and safety are paramount.
- We will ringfence surgery capacity to provide care at scale and reduce delays, managing waiting lists with partners to deliver the best outcomes.
- We will foster a culture of continuous quality improvement, learning, and safety.
Centre of excellence:
Providing the highest quality specialist care and the best possible outcomes for all patients
We will build on our expertise as a centre of excellence, to become a leader in both specialist and general care, ensuring that we remain at the forefront of medical advancements and continue to deliver high-quality care.
- Our excellence shall be underpinned by an ethos of continuous quality improvement, research, and innovation.
- We continue to be an exemplar of the GIRFT principles.
- We will be a provider of high-quality hyper acute and specialist care to our system and beyond, and work with cancer providers to improve care and reduce health inequalities and variation.
Add value:
Using our resources effectively to support services and improve health outcomes
We will be innovative and transformational in providing compassionate, effective and modern care for our patients and population. We will use our resources effectively to improve productivity incorporating wider considerations on how we utilise our estate and how we shape and engage our workforce.
- We will use population health data to effectively plan care and investment.
- We will deliver care in the right setting, appropriate to need, seven-days a week.
- We will use digital technology, AI and data to assist with decision making and for the effective use of our resources
Care without walls:
Providing the right care, in the right place at the right time
We will ensure that we provide the right care, in the right place, at the right time supported by AI and digital technologies, in and out of hospital. This will enable the seamless integration of care across traditional boundaries.
- We will use digitally enable our provider and system partner teams to integrate care.
- We will deliver more holistic care, closer to home whenever possible.
- We will expand, enhance and optimise the use of our virtual wards and remote monitoring, shifting the focus from treatment to prevention.
Our changing context
Lord Darzi described three key shifts to enable us to deliver compassionate, effective, modern healthcare in the future. The shifts focus on moving care from hospitals to communities, making better use of technology, and prioritising prevention over treatment.
- Treatment to prevention: focusing on preventing sickness, not just treating it.
- Analogue to digital: effective use of digital technologies to provide great care
- Hospital to community: shifting care from the hospital setting closer to home
We will be transforming how and where we deliver healthcare over the next five years to achieve our
ambitions. Through our connected care data analysis of our local population, working with system partners
and researching future healthcare opportunities, we have developed large scale transformation initiatives and our neighbourhood working models. These will enable us to deliver compassionate, effective, modern healthcare in the future.
Care embedded in the community and closer to home is about providing care differently but continuing to
provide care that is safe, compassionate and effective.
Our critical transformation enablers will provide the changes in service needed to deliver care in the future.
- System heavy users: Proactive care to holistically manage complex patients within the community could reduce healthcare contacts by more than 10% and improving patient experience. This is closely linked with wider transformation around our aging well strategy.
- Virtual hospital: A multidisciplinary approach allowing reduced length of stay, and reduced bed demand and ward transfers. This will improve patient centred care, through improved access to diagnostics and decision making.
- Acute Medical Unit (AMU): Acute Medical Unit: Adequate bed capacity and clinical resource in our acute medical units and medical SDECs will enable the delivery of high- quality assessment and acute care so that patients who can be treated and discharged in under three days are admitted to the AMU only. Concentrating skills and resources in the AMUs aims to improve the efficiency of care for these patients and benefit the functioning of the hospital as a whole.
- Emergency front door/ admission avoidance: An effective emergency department (ED) and a
clinical operational centre that establishes and directs patients through alternative pathways to ED care that can be delivered in the community, alongside the creation of urgent integrated primary care access points. - Elective recovery: Further develop our GIRFT accredited Heatherwood hospital
to respond to the increasing demand and growth of elective services, particularly high volume/ low complexity work. -
Community beds: To achieve the left shift and right sizing of the new hospital there is essential investment required into 80 additional community beds to deliver care closer to home, both for step-up care as an alternative to hospital, as well as post-illness re- enablement. These will be aligned to “complexity hubs” that will facilitate the assessment and care of multi-morbid patients and their problems.
Our new hospital and how the future of healthcare will be enabled by our people and technology
The national investment in the new Frimley Park Hospital is a once-in-a-generation opportunity to improve healthcare for the communities we serve. This state-of-the-art facility will set new standards in healthcare, integrating the latest sustainability initiatives and cutting-edge digital technology to deliver high-quality services.
Our new Frimley Park Hospital will feature modular and adaptable spaces that can be reconfigured as needs change, allowing quick adaptation to surges or shifts in care needs. Clinical services will be aligned and adjacent to complementary clinical care functions.
Redesigning urgent and acute care is one of our key transformation enablers including the redirection of patients through alternative pathways for urgent care services where appropriate. This will enable our teams to deliver acute care more effectively. We will expand key clinical teams to help us deliver this, such as our acute medical staff.
Biophilic design elements like indoor gardens, green walls, and water features will enhance mental wellbeing.
Sustainable infrastructure, including solar panels and energy-efficient systems, will make the hospital eco-friendly.
We will have enhanced integration and interoperability between critical care and specialist teams.
We will be the best place to work in the NHS, ensuring our people have the skills they require to operate effectively in a digital world; delivering compassionate, effective and modern healthcare. Our people will be encouraged and supported to work across boundaries.
The hospital will serve as a hub for community health programmes, from wellness workshops to preventive care clinics as well as safe, effective high quality joined-up care. This is integral to our critical transformation enablers.
The hospital will provide spaces for staff and patient wellbeing within a relaxing environment.
Our new Frimley Park Hospital will deploy state of the art intelligent hospital capabilities to not only enhance the experiences of both our patients and staff but enable us to integrate with the wider health ecosystem. We will use data (from Connected Care and other sources) and AI to help us deliver compassionate, effective and modern healthcare with the best clinical outcomes.
Education and research are required to support the development of digital literacy and use of Artificial Intelligence within Frimley Health.
Our clinical themes
About our clinical themes
Frimley Health provides a wide range of services across planned and unplanned care, across all ages, delivered across multiple sites.
Continuous quality improvement, research and innovation and education and development underpin our clinical strategy.
Our clinical theme chapters
Clinical engagement workshops were held to develop the clinical strategy in each clinical theme listed below. For each of our clinical themes described, we have included an introduction, a description of the services today, and what the services will look like, and how we will get there, including prioritising initiatives based on coherence, impact and feasibility.
- Urgent and emergency care
- Planned care
- Critical care
- Women’s health, maternity and neonates
- Children and young people
- Cancer
- Specialist services
- Core clinical services
- Ageing well
- Out of hospital care
-
Long term conditions
Our guiding clinical principles
We have described our ambitions according to our four guiding clinical principles:
Firm foundations: Building on our solid foundations for the future.
Centre of excellence: Providing the highest quality specialist care and the best possible outcomes for all patients.
Add value: Using our resources effectively to support services and improve health outcomes.
Care without walls: Providing the right care, in the right place at the right time.
Continuous quality improvement, research and innovation and education and development
Continuous Quality Improvement (CQI), research and education are key synergistic enablers to the delivery of our strategic ambitions.
They are crucial to us creating an environment where healthcare is focused on achieving excellent outcomes, is grounded in the latest evidence-based thinking, is agile to change and proactive in the use of cutting-edge technology.
They will know that developing their skills in these areas will be central to working at Frimley Health and they will be able to access related support and training with ease.
Well-embedded educational programmes result in improved staff morale.
Continuous Quality Improvement
Frimley Excellence is the core cultural principle that permeates all areas of our organisation, from ward to board.
Our approach to CQI - Frimley Excellence (FX) - drives both large and small-scale improvements, with those closest to care playing a pivotal role in identifying and implementing changes. FX has been in place for several years now and a fifth of our people have had training in FX.
Research and innovation
The Research and Innovation (R&I) department supports research delivery across all Trust sites.
Engagement in research is particularly strong in areas such as ophthalmology, urology, emergency medicine and gastroenterology. Across commercial and non-commercial studies there are drug trials, device trials and large observational studies.
We recently moved into the new South Central Research Delivery Network and have academic partnerships with local Universities, with several staff holding academic appointments. In 2024, we commercialised our first Trust-developed medical device.
Education and development
Our Education and Development (E&D) teams strive to ensure that the training needs of our current and future workforce are met by maintaining a proactive approach in response to changing healthcare needs, treatments, and models of delivery.
Well-embedded educational programmes and effective supervision result in improved staff morale and retention rates, as well as reduced sickness and vacancies.
The importance of a structured and supportive educational department is critical in developing resilient and responsive healthcare teams and safer care environments.
We want to simplify and signpost development opportunities to ensure that all staff see CQI, education, research, and innovation as core to their work.
Continuous Quality Improvement - Frimley Excellence
CQI is a key enabler for our long-term ambitions. Our approach equips people with the knowledge and skills to practice CQI in their daily roles, including, problem solving, data analysis, team building, research, digital improvements and enhancements, celebrating success, and collaborating and innovating together.
By fostering a culture of improvement we will ensure that every level of the organisation is engaged in delivering better outcomes. Within two months of joining Frimley Health, staff will complete the Frimley Excellence white belt training and begin contributing to continuous quality improvement initiatives.
Research and innovation
Through Research and Innovation, we aim to:
- Provide dedicated clinical space for research across the Trust to expand capacity and reach across all clinical specialties.
- Integrate research and innovation into business as usual to improve patient access to the latest treatments.
- Sponsor home grown research and innovation to support staff developing their own research portfolios addressing important clinical questions relevant to our patients.
- Strengthen our links with local academic partners
- Lead and innovate in research areas relevant to our patient population.
We will accelerate the adoption of innovation and advancements in healthcare, including artificial intelligence, genomics and robotics, where these can enhance high quality and/or personalised care.
We are committed to innovation through the development of an Innovation Hub, which will streamline the process from ideas to development, commercialisation and distribution, enhancing patient care. It will also provide a collaborative framework for healthcare professionals, researchers and industry partners. We will engage with our regional Health Innovation Networks and industry partners/ universities to support our efforts.
Education and development
We will respond to the changing face, demands, and needs of our future workforce by equipping our clinical staff with the capabilities required to work in modern healthcare. For example, digital competence, use of AI, data science and analytics, use of technology, and agility to work in different spaces.
We will explore data science to support resource and what that should look like, working with our system partners to achieve this.
We will expand our student and apprenticeship offer, develop Frimley Academy to deliver our own professional training, especially in those professions where we see challenges to recruit e.g. across our therapies.
Continuous quality improvement - Frimley Excellence
We will train all our people on the approach to embed a culture of continuous quality improvement across all areas, making improvements based on feedback, data, research, innovation and best practice. This will be achieved through training, coaching, and role-modelling the FX approach. We will work with our system partners to identify a common unified approach to continuous quality improvement to maximise the benefits for our staff and patients across the system.
Research and innovation
We will work with our system partners to prioritise research that will reduce local health inequalities and improve outcomes. There is potential for joint governance and shared resources to enhance our research capabilities.
We want staff to develop their own studies with the Trust as the sponsor. New training resources will ensure staff are confident to support research delivery.
The importance of using evidence and data to shape services and drive decision-making will prompt the need to explore increased data and analytics resources.
Education and development
We will invest in our people through education, training programmes, structured learning, coaching, mentoring and apprenticeships.
A particular focus will be on supporting our people to be more digitally literate.
We will continue to develop a school of health across the Trust and continue to be a positive partner to universities and higher education institutions.
We will develop stronger collaboration with our system partners and the use of local population health data.
We will build in spaces to ensure the needs of modern healthcare education delivery can be met, such as digital training spaces or virtual reality simulation.
Urgent and emergency care
Delivery of effective urgent and emergency care is a critical aspect of effective health services provision.
It is long recognised that urgent and emergency care (UEC) is a system issue that requires sufficient capacity and operational efficiency across all providers involved in delivering care. When the system is challenged by increasing UEC demand, often there is significant impact on staff allocation and resourcing of planned care, resulting in cancellations and delays for patients.
There is a sound evidence base on the effective management of UEC, including attendance management initiatives, streaming patient flows, direct access into assessment units, specific provision for adults, children and patients requiring mental health support and separation of elective work. All are underpinned by senior clinical decision maker models, multi-disciplinary team working, effective training and use of technology and innovation.
Leveraging best practice in these areas alongside the creation of appropriate estate design, resource, digital and patient engagement are critical to create the optimal patient experience in urgent and emergency care.
The Emergency Assessment Centre (EAC) at Wexham Park Hospital is a facility designed to enhance emergency care, although further work is needed to manage patient flow in an optimal way. The EAC includes:
- Emergency Department (ED): This includes single ‘majors’ rooms for seriously ill patients, resuscitation rooms, and assessment rooms. There are also separate areas for children and patients with minor injuries.
- Ambulatory Emergency Care Unit (AECU) / Medical Same Day Emergency care (SDEC): A service that provides an acute service with the aim to provide an alternative to hospital for patients who would ordinarily have been admitted.
- Surgical short-stay beds: Beds for patients requiring short-term surgical care.
Our work starts today to begin improving and transforming how and where we deliver care in the new Frimley Park Hospital. Frimley Park currently has:
- Emergency Department: Located at Frimley Park Hospital and open 24/7, 365 days a year, providing the full range of emergency services.
- Urgent treatment centre (UTC): For less severe injuries, the UTC at Frimley Park offers assessment and treatment for minor injuries like sprains and strains.
- Ambulatory emergency care unit (AECU) / medical same day emergency care (SDEC): that provides an acute service with the aim providing an alternative to hospital for patients who would ordinarily have been admitted.
- Acute medical unit (AMU) – 42 bedded unit with nine enhanced care beds. It offers a multidisciplinary approach to acute medical patients to deliver acute management and optimise length of stay.
Primary and community-led services include urgent Care Centres that can treat patients with less serious ailments without an appointment. Patients can also call NHS 111 for medical advice or to find the best local service to meet their needs, including GP out of hours services.
- We want our patients to have seamless access to the right clinician, in the right place, at the right time, without unnecessary delays or complications. We will structure and stratify urgent care to maximise the use of different resources mobilised to need. We will see and treat 95 per cent of patients within four hours of their arrival in the ED.
- We will provide a consistent service provision throughout the week that ensures compassionate care, with the best possible clinical outcomes.
- We want to create a system that manages increasing demand through innovative strategies, including pre-hospital intervention.
- We aspire to be a healthcare system where both elective and emergency care are prioritised and adequately resourced. We will improve our early (“72-hour”) admission processes. Patients will be able to interact with their medical record and participate in discharge planning. Patients will be able to complete tasks remotely, with technology reducing the administrative burden.
Hospital to community
We will use our connected care data to inform the availability of urgent community and out of hospital care, as well as secondary care advice to primary care.
We will enhance the integration of urgent care services with primary care and community services - exploring opportunities to support primary care at scale across seven days. We will improve estate utilisation by enhancing the integration of urgent care services with primary care and community care.
We will scale up remote monitoring in homes and care homes and virtual care initiatives to provide timely and effective care outside of traditional hospital settings.
We will continue to expand our hospital at home settings at scale and jointly the increase the use of virtual ward spaces.
We will use our estates effectively by the co-locating of same day emergency care, acute medicine, ambulance and direct primary care access with emergency medicine in the new Frimley Park Hospital. All departments will be able to link to a virtual ward environment.
We will work alongside our mental health partners to equip our staff with the skills and knowledge to care for patients with mental health needs when in our care. We will provide adequate mental health resources and improve the integration of mental health and physical health services.
Treatment to prevention
We will use our connected care data to inform proactive care measures and admission avoidance where appropriate, using patient segmentation and remote monitoring to improve efficiency, experience, and outcomes.
We will develop our AMUs and medical SDECs in line with the Society for Acute Medicine (SAM) and GIRFT recommendations to align with our demand. We will ensure adequate resource and workforce to the AMU, SDEC and assessment areas to optimise the acute care for patients for up to 72 hours and aim to provide a consistent service throughout the week.
Acute medical units (AMUs) are rich learning environments for a wide range of health professionals and students. We will ensure a focus on this, given high-quality teaching and learning have a direct impact on patient safety, quality of care, and the experiences of our workforce.
We will provide comprehensive care for mental health patients, clear operational processes in place, fully utilising therapy skill set and capability in UEC pathway.
Analogue to digital
We will use our Connected Care information across providers, to inform how, where and we deliver care.
We will create new platforms for regular discussions between primary care physicians and secondary care consultants, fostering in-reach from social services.
We will maximise the use of digital technology, through MyFrimelyHealth Record, remote monitoring, AI and other innovative technologies.
Planned care
Frimley Health is a recognised provider of high-quality elective care and has been able to attract high-calibre clinicians to lead its services. It has achieved national GIRFT accreditation and regional recognition for its planned care work at Heatherwood Hospital.
In the post-Covid era, there remains significant national focus on access to elective care to address long waiting lists and sometimes inequalities that have emerged.
The Heatherwood Hospital elective centre has demonstrated the benefit of elective and non-elective separation of care.
However, when faced with complex procedures and patients, our acute hospitals need to further evolve their physical layout and staffing models to improve productivity, efficiency, and patient satisfaction. The adoption of digital and AI solutions, several of which have already been rolled out, provides an unprecedented opportunity to further support these aims.
Further work is also needed on delivering the best access, diagnosis, early detection, and outcomes in cancer services, which remain a collaboration with specialist partners from outside our integrated care system.
We are also aware of current and projected challenges in recruitment due to national workforce shortages, such as anaesthetists and in cohorts of our workforce approaching retirement. Maintaining specialist focus and a modern healthcare environment is key to recruitment and retention.
We are proud of our delivery of local planned care services across our hospital sites at Frimley Park, Heatherwood and Wexham Park and our community sites.
Our planned care services span outpatients, diagnostics and inpatient care, and our specialties include: cardiology, orthopaedics, general surgery, gynaecology, ophthalmology, dermatology, ear, nose, and throat (ENT), plastic surgery, gastrointestinal and liver services, urology, vascular surgery, endocrinology and metabolic medicine, neurology, rheumatology, pain management, respiratory medicine, including cystic fibrosis and sleep medicine.
Renal medicine in partnership with St Helier Hospital increases access for local renal patients requiring renal vascular access and renal dialysis care without transfer to London.
Our elective hub was in one of the earliest accreditation waves of the GIRFT hub programme and has been recently re- accredited. It has showcased care to governmental and regional staff responsible for co-ordinating healthcare, and specialities such as ophthalmology have been used as national exemplars.
Reduced waiting times and health inequalities, improved life expectancy and equality of access, with a focus on both prevention of chronic illness and related complications. We want to maintain and build-on key specialist services, providing enhanced and expert care for our patients and enabling us to attract and retain leading clinicians in their field. We will deliver treatment to 92% of patients within 18 weeks of being referred to us.
Our care and access to it, to be revolutionised by the power of digital, genomics and AI, while remaining grounded in our core philosophy of outcome-focused, evidence-based, safe, and personalised care. We will be at the forefront of digital innovation and new technologies.
We will continue to improve the primary to secondary care interface. We will have new complexity hubs for patients with multimorbidity associated with aging, that will reduce duplication and promote holistic care. These should be linked to community diagnostic centres. We will expand our virtual wards, multi-disciplinary working and further integrate them into urgent care assessment points and remote monitoring services. We will increase our ‘one stop shops’ approach.
We will provide flexibility in appointment times and sites, with elective services across seven days and evenings to improve access, patient satisfaction, and estate utilisation. Through MyFrimleyHealth Record, our patients will be able to manage their appointments and have access to up to date, accurate, easy to understand information. Our patients who are not able to access information through digital technologies will have easy access through other communication channels.
Hospital to community
We will ensure separation of elective and non-elective care to maintain effective use of our facilities. We will expand Heatherwood as an elective powerhouse to manage elective workflow and maximise capacity. We will create a specialist elective wing on the new Frimley Park Hospital, and existing Wexham Park site. We will expand our intensive care and high dependency areas to support the best outcomes through enhanced recovery and care for complex surgery.
Through our community diagnostic centres we will provide wider access to tests and diagnostics in the community to champion a community first approach, while also increasing opportunities for one-stop pathways.
We will have more targeted outpatient appointments delivered in the community and rapid access to advice and guidance, providing joined up care with primary and community services.
We will continue to expand the use of our virtual wards and multi-disciplinary working.
We will develop a workforce that can provide cover for elective as well as non-elective weekend and evening working. The Trust has already reached six-day elective services in key areas and our Heatherwood elective hub.
Treatment to prevention
Where it is clinically appropriate to do so, we will redevelop outpatient services to provide advice and guidance, reducing the need for patients to attend appointments, while also continuing to optimise the use of patient initiated follow up (PIFU). MyFrimleyHealth Record will provide direct booking options to patients, reducing non-attendance (DNAs).
We will develop complexity hubs for patients with multiple conditions associated with aging, reducing duplication of outpatient appointments and promoting holistic care. We will also improve productivity through enhanced pre-operative assessment, minimising unplanned elective cancellations, thus allowing patients faster access to elective slots.
We will identify patients most at risk or with the greatest needs to provide preventative care where possible. We will reduce health inequalities, enable prevention and self-management, maximise screening and early intervention.
Our GIRFT programme has and will continue to reduce waiting lists by embedding best practice and delivery of rapid clinical transformation and efficient patient pathways.
Analogue to digital
We will expand virtual wards supported by digital technologies and AI. Building on successes in clinical AI transformation, like ophthalmology, improved scheduling, digital wayfinding, advanced virtual wards, and consultations.
We will continued to optimise our trust wide electronic patient record system to support clinical audit and recording outcomes, as well as modules to increase patient engagement and control via MyFrimleyHealthRecord. This will be available in different languages for better accessibility. We will also offer alternative communication channels for patients who cannot access information digitally.
Critical care
Our critical care services support our sickest patients and seek to achieve the highest levels of health and independence after severe illness or injury. Where interventions have been unsuccessful this role turns to supporting compassionate end of life care for patients and loved ones, and where applicable, the crucial role of organ donation and transplant.
Critical care faces significant challenges. The demand for critical care beds has increased by over 10% in the past decade, with increasing complexity of both planned and emergency admissions. Future pandemic planning, with suitable environments to cope with such surges, has also prompted review of critical care services on a wider regional and national scale.
Our critical care services provide level three and level two care at Wexham Park and Frimley Park Hospital, admitting both emergency and elective (planned) patients who need critical care support. The Frimley Park intensive care unit (ICU) also provides critical care for specialist services such as vascular surgery, hyperacute stroke, interventional cardiology, and cystic fibrosis. Both ICUs are supported by a post anaesthetic care unit (PACU) to allow recovery post anaesthetic and short-term augmented care to be delivered outside of critical care.
The Trust has invested in 24/7 rapid response teams to support both critical care units, and comprise trained nurses, advanced nurse practitioners and ICU consultants. These teams work in an outreach capacity to support acutely unwell patients in the acute hospital at risk of deterioration to a point of requiring critical care input/admission.
These teams also support patients in the step down from an ICU stay back to the wards, and were early adopters of Call4Concern patients or families can self-refer into the service.
ICU follow up-clinics work alongside critical care rehabilitation services on each site, with clinical disciplines collaborating to ensure that ICU care continues into the recovery phase of critical illness. These services have a strong evidence base for optimising recovery and reducing long term morbidity, and we will seek to continue to ensure that these can be accessed by all
would benefit.
Our critical care units work in partnership with a separate medical acute dependency unit (MADU) and surgical acute dependency unit (SADU) located on each acute site. These are run by the respiratory physicians and general surgeons respectively, and provide level one, and selected level two care. These partnerships have helped our critical care teams respond to sustained pressure and ongoing capacity challenges and will form part of our provision moving forward; however, the ability to flow patients through these units according to need is affected by wider general capacity constraints (step-down), and growth in critical care beds needs to match accordingly.
Despite these challenges, our critical care teams report good quality indicators, which highlight their dedication and resilience. Our workforce has also faced significant strain, with a particular focus needed on retaining our experienced staff and managing the psychological burden of these roles. This can be improved through education and development. Digital innovation that uses clinical measures to optimise clinical pathways, such as the identification of deteriorating patients, are already in place.
We want to develop a flexible and resilient service that responds to immediate and urgent need, but also places greater investment in the prediction and prevention of critical illness, using clinical data to help inform outcomes. Our patients and their families will be involved in designing our services through capturing and using their lived experience.
We want to be a critical care service that is compassionate and focused on providing high-quality, patient-centred care for the populations we serve, continuing to maximise functional recovery and outcomes though both critical care, discharge and rehabilitation.
Multidisciplinary teams, inside and outside critical care, will work efficiently and seamlessly to manage complex cases and share clinical responsibilities, supported by the latest technologies, therapies and treatments.
The suite of specialty services at Frimley Park is such that we will look to co-locate several specialist high-dependency units in the new Frimley Park Hospital to ensure the most effective clinical collaborations and outcomes. We want to ensure future sustainability of the critical care workforce across all professions so that we continue to have confidence that we will have the right staff with the right skills to care for the critically sick patients in our organisation.
Optimising pathways and transitions
By ensuring that patients receive the right level of care in the right environment their needs, we will improve outcomes and reduce the pressure on intensive care units.
- By ensuring patients receive the correct level of care in the most appropriate clinical environment (ward, MADU, SADU, hyper-acute stroke unit (HASU) or coronary care unit (CCU) for their needs, we will improve outcomes and reduce pressure on the intensive care units (ICU). This will be underpinned by existing and emerging digital/AI tools to segment the risk of deterioration in the wider hospital, and before major planned surgery.
- We will plan to co-locate our higher dependency units (ICU, MADU, SADU) at the new Frimley Park Hospital, which will give us an opportunity to manage the correctly sized bed base, flex according to need (such as seasonal variation) and share relevant staffing expertise.
- We will manage regional service pressure by working with both Wexham Park and wider network partners to enhance access to critical care services, reduce delays, and maintain our specialist (tertiary) services.
- We will achieve our ambition to reduce discharge delays from ICU as this will have an impact on overall ICU capacity and allow us to be more responsive.
Analogue to digital
We will harness emerging AI technology to analyse patient data and predict potential deterioration or readmission risk on wards, therefore enabling pre-emptive clinical intervention, which will contribute to a safer and more efficient critical care environment.
We will use digital support in the follow-up care used by our rehabilitation tracking after intensive care unit discharge, facilitating seamless transitions, monitoring for long-term recovery and outcomes.
Other enablers
We will co-locate higher dependency units (intensive care unit, MADU, SADU at the new Frimley Park Hospital.
We will provide structured career pathways and development opportunities to attract and retain the best and most experienced staff.
We will develop the complex multidisciplinary workforce needs, by working with higher education institutions (HEI) and other partners to strengthen the pipeline into critical care roles and review the totality of the workforce to identify opportunities for more effective care delivery.
We will develop the future critical care team and look at how administrative and support roles can reduce workload burden, alongside digital innovation.
We will prioritise patient recovery and long-term wellbeing through integrated and structured rehabilitation and follow-up care, supporting patients’ transition from intensive care to full recovery. This will include enhanced mobilisation and rehabilitation within the ICU, post-discharge support onto the wards and then community, and holistic care, including linking with social workers and community partners.
Women’s health, maternity and neonates
Our approach to caring for women and their babies today is crucial for building healthier families and communities tomorrow. We will ensure that our services provide responsive care from birth up to and including healthcare transition into adulthood.
Providing the right care, in the right place, at the right time throughout life to women and during pregnancy, birth, and the postnatal period lays the foundation for lifelong health and wellbeing. By ensuring that women and babies receive high- quality, accessible care, we create the conditions for a stronger, healthier population and a more resilient healthcare system.
The health of women and babies in the UK reflects both remarkable progress and persistent challenges. Maternal mortality has decreased significantly over decades, yet inequalities remain stark.
Women from Black ethnic groups are still nearly four times more likely to die during pregnancy or childbirth compared to White women, and women from deprived areas face higher rates of adverse outcomes. Meanwhile, around 10% of infants in the UK require readmission after birth.
Our maternity services received a ‘Good’ rating in 2023 from the CQC and has met all the required safety standards for the Clinical Negligence Scheme for Trusts.
We will emphasise early intervention for maternal conditions such as diabetes and hypertension, promoting lifestyle changes like diet and exercise to reduce future health risks.
Our women’s health services are comprehensive, covering community, emergency, elective (planned), outpatient, and specialist provision, including gynaecology, maternity, obstetric, and neonatal services. These services are available across our main hospital sites and community hubs.
We care for approximately 9,500 expectant mothers each year, working collaboratively with our local maternity and neonatal system (LMNS) and Maternity and Neonatal Voices Partnerships (MNVPs). We provide 132 hours a week of dedicated consultant delivered care on the both our labour wards. Our services include two co-located midwifery led birthing centres. Our maternity hubs, located close to family homes, provide support and continuity during pregnancy and after birth. We aim to expand this model, ensuring our workforce and facilities are fit for the future.
We have one of the lowest rates of unplanned admissions to neonatal units in the region, thanks to improvements in maternal health and the Saving Babies Lives initiative. Our maternity units focus on keeping mother and baby together, which has led to the success of our transitional care units.
There has been a significant rise in caesarean section rates, reflecting a national trend and increased emphasis on women’s choice in maternity care. This trend has implications for service provision and staffing, which must be considered in long-term planning.
We provide comprehensive gynaecology emergency outpatient and inpatient services including an ambulatory service and are a specialist Endometriosis Centre. Our pelvic health service is a national trailblazer.
- We will enhance the delivery of care to ensure services are responsive, patient-centred, and accessible. We will address inequalities in access and engagement, for example improving outcomes for mothers and babies from minority ethnic groups. We will continue to build on the success on our telephone triage MAMMA’s Line.
- We want to be a high reputation service for women’s health, delivering excellent, local gynaecology, maternity, and neonatal services designed around the population health needs, where women feel supported and listened to as active partners in their care. We want to address disadvantage and the inequalities that are prevalent across our populations to ensure families experience better starts, better health, and excellent outcomes.
- We will promote sharing information digitally through the maternity website, that is accessible to our population and provides a digital antenatal education platform. To provide personalised care through digital access, working towards a fully accessible integrated single electronic patient record.
- We are committed to improving postnatal support to ensure the long-term health and wellbeing of mothers and newborns. According to the Royal College of Paediatrics and Child Health (RCPCH), enhancing postnatal care could significantly reduce the risk of readmission for newborns.
Hospital to community
Care closer to home: We will expand and future proof our maternity community hubs, ensuring we have the right staff in the right place embedded in our communities to deliver multidisciplinary care including pelvic health and mental health as essential to longer term wellbeing.
We shall explore opportunities for enhancing community-based gynaecology services with primary care partners centred on avoiding the need to be on a hospital site for diagnostics or treatment unless necessary.
Our targeted outreach programmes and community engagement initiatives will aim to improve access for underserved communities.
We shall be innovative in this approach exploring all options including ‘care on the high street’.
We will strengthen current emergency services e.g. same day emergency care (SDEC) and ambulatory care.
Treatment to prevention
We will ensure strategic planning to anticipate major clinical changes e.g. increasing the use of biologics for gynaecological conditions and reduction in some surgical interventions
as a result.
- Maternal medicine and long-term health: We will work with specialist maternal medicine partners on the complexity of multiple medical conditions presenting in pregnancy to ensure responsive joined up services with excellent outcomes, that are as close to home as possible. We will address health disparities and promote preventive care through outreach and education.
- Maternal mortality: We will be aligned with the local maternity and neonatal system (LMNS) to understand our population health data and ensure that initiatives aimed at understanding and mitigating maternal health disparities, particularly women from ethnic minorities, will be prioritised to improve outcomes and reduce mortality rates.
- Preventive care and population health: We will emphasise early intervention for maternal conditions such as diabetes and hypertension, promoting lifestyle changes like diet and exercise to reduce future health risks. Special attention will be given to supporting healthy ageing, particularly in older women. We will ensure a skilled, resilient workforce to meet current and future healthcare needs.
Analogue to digital
We will use population health data to drive evidence-based decision making to enable us to deliver compassionate, effective and modern care to our local population. We will leverage technology and co-designed care models to enhance patient experience and accessibility.
- Education and support: Centralised, data-driven platforms will provide reliable health information to combat misinformation and empower individuals to manage their health proactively.
- Choice and personalisation: The effective resource allocation will focus on supporting personalised care options and shared decision making, empowering patient autonomy and decision- making within their treatment paths. We will use advanced tools like AI-driven translation, mobile health apps, patient portals, and virtual tours to help overcome language barriers, provide timely information, and create a more inclusive care experience.
Other areas
We will focus on reducing the significant back log for planned care. We are aligned to the three-year delivery plan for maternity and neonatal services 2023 and continue to work towards the delivery of the LMNS perinatal equity and equality five-year plan. We will focus on maternal and neonatal care that prioritises inclusivity and positive outcomes for all.
Children and young people
Our approach to caring for children and young people is fundamental to a healthier and stronger tomorrow. Ensuring the right care and preventative approaches are delivered in the right place, at the right time lays the foundation for a healthier, more resilient adult population in the future.
By addressing the health needs of children and young people today, we not only set them up to succeed in life but also uplift the overall health and wellbeing of our communities for generations to come - starting well is vital.
To address the challenges facing children and young people today requires us to tackle enduring health inequalities. Conditions such as obesity, asthma, and type two diabetes continue to rise, disproportionately in children from socioeconomically disadvantaged backgrounds. The burden of respiratory illnesses is likely to increase due to climate change, with children from deprived areas often more exposed to air pollution and other environmental risks.
Mental health issues now affect one in six children aged five-16, an alarming increase in recent years and access to timely mental health support remains inequitable across the country. The investment in children and young people mental health liaison services during 2024 has seen huge successes in providing timely access to support for children in crisis.
Tackling these issues effectively requires a system-wide approach, recognising the interconnectedness of education, housing, healthcare, and the wider social determinants of health. Our paediatric teams will work closely with system partners on shared priorities to reduce health inequalities empowering children and young people to live healthier, more fulfilling lives.
We will develop a fully integrated model that links acute and community paediatric services, ensuring continuity and consistency in care delivery.
The children and young people’s service delivers comprehensive services for local children and young people. These services span hospital and community, providing care in response to emergency and elective (planned) requirements, within dedicated child- friendly environments.
Our children and young people’s services include:
- Acute and general care including neonatal care, paediatric emergency departments, paediatric assessment units, paediatric medicine and paediatric surgery.
- Chronic and complex care including cystic fibrosis and epilepsy.
- Diagnostics including allergy care and phlebotomy.
- Medical specialties including cardiology, community paediatrics, dermatology, diabetic medicine, endocrinology, gastroenterology, haematology, immunology, infectious diseases, neurology, oncology, respiratory, ears, nose and throat and rheumatology.
- Surgical specialties including ophthalmology, orthopaedics, plastic surgery, and urology.
- Outpatient and community teams.
- Level two paediatric critical care unit at Wexham Park In addition, they also collaborate closely with Child and Adolescent Mental Health Services (CAMHS), developmental paediatrics (e.g. autism spectrum disorders (ASD), ADHD, learning disabilities), psychological medicine, safeguarding, speech and language therapy (SLT), as well as our associated clinical networks.
- We will continue to work with system partners to reduce the health inequalities that persist within our populations and using population health data ensure that our services match the needs of our children and young people, collaborating closely on CORE20PLUS 5 (asthma, diabetes, epilepsy, oral health and mental health). We will adapt and accommodate how we deliver care for our patients with additional needs. We will develop our service to deliver high quality, high dependency care to our patients when they need this treatment.
- We will build on our positive reputation and establish our identity as a leading local provider of neonatal, children, and young people’s services, delivering excellent access and outcomes with an emphasis on prevention and engagement.
- We will have pathways of care that are co-designed around the needs of our children and young people and their families that encourage self-management, are supplemented by digital innovation, and keep the child at, or as close to home wherever possible. We will create a virtual children’s hospital within Frimley Health to facilitate a better focus on children and young people’s healthcare, looking after our future generations. We will ensure that our services provide responsive care from birth up to, and including, healthcare transition into adulthood. We will maximise the use of our EPR and MFHR to engage and care for our children and young patients.
- This will include a particular focus on healthcare transition for adolescents and young people with complex needs and/or long- term conditions whose care will move from children to adult services. The children and young people under our care will have timely access to treatment, and those waiting for planned care will be identified so that their waiting time can be minimised with a clear improvement trajectory.
Hospital to community
We will continue to ensure that an inpatient stay for children and young people is the exception and provide care models that support family involvement and wellbeing. We will continue to formalise and build on our ambulatory care and virtual ward models.
We will continue to invest in the children and young people mental health liaison services and evidence the success of this interagency working and further develop the links and cross organisational working.
We will develop a fully integrated model that links acute and community paediatric services, ensuring continuity and consistency in care delivery.
We will increase the availability of local care through outreach clinics and visiting specialists, reducing travel burdens while maintaining safety for complex cases. We will create integrated and seamless healthcare transition pathways for children with complex needs, ensuring smooth handovers between care teams. Our children and young people will have access to community care, for example community diagnostic centres.
We will improve healthcare transition pathways and outcomes (preparing for adulthood), ensuring personalised plans starting at age 14 with collaboration of wider services.
Working with our system partners we will explore the use of talking therapy services across the Trust with a focus on supporting children and young people with long-term conditions.
Treatment to prevention
We will continue to work with system partners and networks to reduce the health inequalities using population health data ensure that our services and staff match the needs of our children and young people.
We will focus on prevention and early intervention, including programmes like complication from excess weight clinics (CEW) and linking care to mental health services. We will also leverage population health data to identify trends and design responsive, preventive services. Our paediatric teams will be linked into the system-wide CORE20PLUS5 work.
We will pilot key worker models to provide consistent support for those with complex care needs and their families. Furthermore, we will work with young healthchampions to incorporate their feedback and ideas into long term condition pathways and adolescent services. We will re-establish the Youth Forum and embed co-design as a core principle across all service developments will ensure our services align with user expectations and requirements.
We will develop a dedicated plan for children’s elective care, separating their waiting lists from overall hospital lists to ensure transparency and focus on improvement. This will ensure that children and young people waiting for planned care are clearly identified so that their waiting can be minimised with a clear improvement trajectory.
We will improve healthcare transition pathways (preparing for adulthood), ensuring personalised plans starting at age 14 with collaboration of wider services.
Analogue to digital
We will expand the use of AI and other digital technologies to enhance tools like “Healthier Together,” ensuring proactive self-management support.
We will invest in telehealth infrastructure to provide flexible, accessible, and high- quality remote consultations for families.
We will develop user-friendly portals to support adolescents and children in managing their health and care pathways.
Other enablers
When admission is required, our new Frimley Park Hospital will provide exemplar accommodation for children and their carers and be an aspirational exemplar for future NHS care.
We will explore and develop adolescent- friendly areas within wards, focusing on creating supportive environments tailored to the needs of this age group.
Cancer
Frimley Health diagnoses cancer in around 500 people every month, and approximately 3.1% of our integrated care system population is living with cancer - with many having ongoing treatment. Cancer survival in England has lagged behind similar nations for many years. We are committed to addressing this in our area by providing the best local cancer services in the NHS.
To support improving the national position, the current long-term plan asks the NHS to improve the proportion of patients diagnosed at stages one and two from 50% to 75%. For our population this is currently at 64% There is also a need to reduce variation and ensure the most up to date treatments are available for all appropriate patients as quickly as possible. The challenge for us is to make improvements in cancer survival and patient experience, in the context of several broad issues including:
Population growth
The growth in population has led to increased overall demand for cancer treatment and care.
Ageing population
An ageing population has resulted in more cancer being diagnosed that may be amenable to treatment. The elderly population also has higher potential for having multiple illnesses or conditions, adding to the complexity of diagnosis and treatment.
Increased availability of treatments
The availability of new and advanced treatments has resulted in increased demand for cancer services. As technology advances, more patients are seeking treatments that were previously unavailable or inaccessible. The costs of these new treatments in terms of additional infrastructure, equipment, workforce and medicines are a significant challenge.
Rising demand for cancer care related to lifestyle
Obesity, diet, smoking and alcohol consumption are significant risk factor for cancer which are driving increases in cancer incidence.
Our Trust has an excellent record of cancer care, delivering outstanding times to diagnosis and treatment, clinical outcomes, and patient experience. Recovering from the effects of the pandemic remains a challenge which are being addressed.
Survival and outcomes and inequality
Our cancer survival rates overall are better than the England average for all tumour sites and continue to rise, but we recognise that some populations have far worse outcomes. We are looking to address the inequalities across our geography.
Prevention, screening, and earlier presentation
We provide breast cancer screening for some of our population. We are also leading the rollout of lung cancer screening and collaborating to provide bowel, breast, lung health (lung cancer), colonic and cervical cancer screening services. Staff work with partners to increase people with potential cancer coming forward.
Waiting times for diagnosis and treatment
Waiting times for diagnosis and treatment remain a challenge in some specialties. Recent significant improvements are being built upon to return to top 10 performance.
Patient experience
There has been some excellent feedback though the National Patient Experience Survey. There are areas for improvement, which are being worked on.
Capacity
Capacity overall remains good but matching capacity to demand growth requires work for some tumour sites.
Workforce
The Trust attracts a high calibre workforce and regularly reviews skill mix to improve access.
Research and innovation
The Trust has led the way in several areas particularly renal, urological and bowel cancer treatment.
- Our staff skills and capacity will be developed in order to meet the rising demand for cancer care. We will deliver greater direct access to diagnostic tests by primary care clinicians. We will increase our cancer prevention activities and deliver new or enhanced screening and surveillance programmes.
- We will reduce the time it takes to diagnose and treat cancer, delivering cancer wait times performance in the top decile in England. We will develop services to ensure they can provide the most up to date cancer treatments. We will increase participation in cancer research and development. We will utilise new technologies such advances in AI, supported by our electronic patient record.
- We will work with partners to deliver more prevention activities. We will deliver more cancer treatment and care closer to, or in the patient’s home. We will increase provision of more personalised care through higher levels of holistic needs assessment and care co-ordination. We will deliver higher levels of excellent end of life care for cancer patients at the place of the patient’s choice.
- We will improve our cancer patients reported experience of care and quality of life. We will further increase cancer survival, reducing inequalities of access, experience and outcomes. Together with our education academy we aim to generate future income (for example through our cancer care module and webinars).
Hospital to community
Travelling for treatment is a significant physical, emotional and financial burden for patients with cancer. We want to reduce this as much as possible by delivering more care closer to home, ensuring that there is enough investigation capacity. We also want to provide more systemic anti-cancer treatments, that patients currently receive at tertiary centres, locally.
As our relationships with tertiary cancer centres develop, we will work to ensure patient pathways involve as few touch points and as little travel as possible, ensuring the best patient experience we can.
Our improved multidisciplinary team working and remote consultation will ensure effective use of resources. We will develop our people, ensuring a workforce able to deliver excellent cancer care, now and in the future.
We will maximise new cancer pathways developed in our elective hubs (GIRFT recognised one stop clinics), continually reviewing opportunities to deliver systemic anti-cancer treatment in patients’ own homes.
Collaboration across our system is an integral part of how we deliver cancer services, and we will continue working closely with GP leaders, NHS partners, public health and third sector organisations (e.g. Macmillan Cancer Care and Cancer Research UK) to ensure ongoing cancer care improvements. We will also continue working across primary and secondary care through the clinical leaders’ forum, and with our key partner the Surrey and Sussex Cancer Alliance.
Treatment to prevention
We are committed to delivering and developing high quality cancer screening and surveillance services for our population. We will increase screening uptake and early referrals for symptomatic patients to improve their stage at presentation and increase cancer survival rates
Specific programmes:
- We will continue to develop and deliver cancer screening and surveillance services, providing a full and seamless lung cancer screening pathway.
- We will build on our experience with the targeted prostate health check programme ensuring that it leads on delivering any new NHS cancer screening programmes.
- We will step up our primary and secondary prevention activities in partnership with system colleagues, using the making every contact count (MECC) approach and leveraging opportunities with MyFrimleyHealth Record.
- We will use our population health database to target education and uptake initiatives in low-uptake groups, and to identify and educate those with poor outcomes to improve results.
- We will review opportunities to improve facilities for patients, delivering holistic care through their cancer journey, ensuring enough capacity to increase care, in particular systemic anti-cancer treatment, closer to home as much as possible.
- We will look to further develop our cancer information centres, participating in initiatives such as the aspirant cancer career and education development framework (ASCEND).
Analogue to digital
We will ensure that the benefits our electronic patient record is capable of, are maximised for patients. This includes greater use of patient self-management, patient information and education provision, support for patients with communication and language barriers and releasing time to care through more efficient ways of working.
We will be at the forefront of implementing AI solutions to improve care. Trust staff have been developing AI technologies in breast cancer screening. We will use population health analytics to inform work to support cancer prevention and ensure outcome variation is continually addressed.
We will agree referral pathways and processes with system partners, minimising delays and repetition within referrals. We will implement electronic referrals with best practise pathways to enable triage to the most appropriate assessment and treatment.
We will review surgical treatment capacity, increasing it as needed to meet rising needs, including where appropriate wider use of surgical robotics and other technologies.
There is a 24% predicted National shortage of clinical oncologists in the next three years, so we need to shift our workforce models and the development of new roles e.g. nurse led services like our acute oncology services (AOS) and the virtual AOS consultant model (at Frimley Park Hospital). We will ensure future clinical staff skills are mapped, and appropriate plans are in place to develop staff to meet these needs. Staff will be developed to support non-clinical care co-ordination, freeing up more specialist clinical time.
Specialised services
The transition of specialised service commissioning to local integrated care systems represents a pivotal moment. This is part of the long-term plan to give integrated care systems the opportunity to embrace this change, and design services that are more responsive, equitable, and impactful. Through collaboration, innovation, and strategic investment, we will position our system to deliver outstanding specialised care for our communities and beyond.
Integrated care system commissioning will empower us to improve patient health and care, by supporting joined up care, and providing the opportunity to focus on population management, improving the quality of service, tackling health inequalities and ensuring best value.
The Trust has also worked in partnership with the Ministry of Defence (MoD) for over 20 years, caring for these patients in the dedicated MoD hospital unit at Frimley Park Hospital, as well as utilising their MoD personnel as part of our workforce. There has been an increase in MOD referrals to the Trust.
The planning, contracting, and design of specialist services is undergoing significant transformation at a national level.
From April 2024, responsibility for the commissioning of most of these services will transfer from NHS England to local integrated care systems. This change provides a unique opportunity to align the design and delivery of specialist services with local needs.
For us locally, this shift opens avenues to:
- Enhance local responsiveness: Tailor services to better meet the needs of our diverse communities, including early diagnosis of certain conditions, such as renal patients.
- Innovate care models: Implement new approaches that improve outcomes and efficiency.
- Leverage new infrastructure: With the proposed new hospital within five miles of the current Frimley Park Hospital, we can reimagine the role specialised services might play, not only for local residents but also for those beyond our integrated care system boundaries.
To navigate these changes and maximise the opportunities they present, we will concentrate on the following areas.
Collaboration with our integrated care system and the Regional Commissioning Hub:
Engage in strategic discussions to integrate emerging regional priorities into our local strategic plans. Ensure alignment with national and regional goals while advocating for the needs of our communities.
Strategic priorities for specialised services:
As the regional architecture evolves, we will remain responsive to opportunities for service redesign and local commissioning which are emerging from this strategy.
Influence the development of regional priorities to reflect the specific health needs of our population.
Key specialised services for Frimley Health include: renal, cancer, cardiology, vascular, cystic fibrosis and stroke.
- Develop a comprehensive local strategy for specialised services in partnership with our integrated care system and regional stakeholders.
- Pilot innovative care models that align with national policy and regional priorities, sharing lessons learned across our integrated care system.
- Establish Frimley Park Hospital as a hub for high- quality specialist care, with capacity to serve both local and regional populations.
- Measure success through improved access, patient satisfaction, and clinical outcomes.
Treatment to prevention
Design and deliver specialised services that are responsive to the unique health challenges and demographics within our integrated care system.
Invest in state-of-the-art facilities that support the delivery of specialised services within the new Frimley Park Hospital.
We will optimise the role of the new hospital by using the new facility to strengthen our position as a potential provider of choice for some specialised services. We will design services that maximise the hospital’s potential to serve both local residents and those from our neighbouring system partners.
Devolution of specialist services is likely to expand demand on renal care and provide local access to advanced techniques such as TAVI, for which we already have the relevant clinical expertise. This will require upskilling of our people.
These will be delivered in an integrated manner for the whole system, whilst managing access to local services for the north and south of the integrated care system in the two acute sites
Hospital to community
Explore opportunities to lead the provision of some specialised service developments across our integrated care system boundaries where it makes strategic and clinical sense.
Position ourselves as the preferred local provider for specialised service pathways that can be unbundled from tertiary centres.
Retain more activity locally, reducing the need for residents to travel to out-of- area tertiary centres for care.
We will develop specialist roles and training programmes to equip staff with the expertise required for expanded service delivery. We will attract and retain talent by positioning our integrated care system as a leader in innovative, patient-centred care.
Working with our system partners and the regional hub we will establish commissioning arrangements that support local delivery while ensuring high standards and financial sustainability. We aim to foster partnerships to build capacity and expertise in areas where shared leadership can enhance service delivery.
Analogue to digital
Invest in digital tools that support the delivery of specialised services within the new hospital.
Use robust data analytics to monitor service performance, identify gaps, and guide strategic decisions.
Use population health data to prioritise services that have the greatest impact on local health outcomes.
Ensure interoperability with regional and national systems to facilitate seamless patient care.
Core clinical services
Our core services are critical to and embedded within all our clinical areas. They ensure patients are diagnosed earlier and receive the right care, in the right place, at the right time.
Our core clinical services include:
- Diagnostics: imaging, pathology and blood sciences, and physiological sciences
- Mortuary services
- Therapies
- Pharmacy
Several challenges are highlighted locally and nationally:
- Growing demand across all diagnostic and core clinical services
- Static rates of early (stage 1 or 2) cancer diagnosis
- Long waits for musculoskeletal problems, which are one of the biggest causes of long-term ill health
- Antimicrobial resistance rising globally and will be one of the major challenges facing future healthcare
In line with the left shift principles, our core clinical services will enable us to deliver more care in the community, focus more on prevention and have a modern approach to how we deliver care through digital integration and innovation.
Reflecting the national picture, our core clinical services cite an ever- increasing demand with capacity and infrastructure struggling to keep pace. There are areas, such as therapies and pharmacy, where seven-day working isn’t presently resourced but would contribute to
improved outcomes and experience.
Pharmacy
Our services provide medicines optimisation and medicines management alongside care delivery which is crucial to effective outcomes.
Therapies
Our service delivers outpatient and acute care to a diverse group of patients using the highly specialist skills across 6 professions. The team are integral to reducing length of stay and optimising patient outcomes.
Pathology
We are proud to host the Berkshire and Surrey Pathology Services (BSPS) Network who carry out circa 55 million tests per year across the whole spectrum of pathology testing. The pathology network is currently provided by a hub- and-spoke model supporting the consolidation of services. We provide mortuary provision on each acute site with the ability to balance the service at times of peak demand.
Diagnostics (imaging and physiological sciences)
There is continued growth in demand for diagnostic radiology and physiological diagnostics. We are investing in additional Community Diagnostic Centre capacity to support faster access and diagnosis away from the acute sites. These are aligned to key pathways and prevention to screen for key health conditions and provide better access to treatment.
- Our core clinical services will be integral to delivering better outcomes for our population. We want to be one of the best performers for our core clinical services in the country in terms of access and reporting times with the aim of hastening diagnosis and treatment and ultimately outcomes.
- For therapies, we will deliver care driven by GIRFT standards, NICE recommendations and national best practice. We will have a focus on prehabilitation as well as rehabilitation. We will develop smoother transfers of care across acute/community boundaries.
- There will be close working across MDTs and consideration given to the impact on these core services whenever transformation or new models of care are being considered. We shall provide more diagnostic options close to patients homes.
- Our system pathways will reduce duplication and reduce the need for onward referrals to secondary care, redesigning historical pathways to optimise outcomes and experience. We aim to future-proof services to address demographic change, rising demand, and evolving healthcare challenges. We will focus on the right test at the right time, reduce duplication and achieve high quality outcomes.
Treatment to prevention
- Pharmacy
Pharmacy to develop new roles for the changing clinical landscape, including consultant pharmacist pathway, clinic-based pharmacists and medicine management assistants. This includes how the service should be delivered over 7 days. Our teams will have capacity to focus on medicine optimisation as a key intervention in preventing adverse outcomes.
We will review and develop pharmacy aseptic medicines preparation service fit for the future which includes increased participation in clinical trials. - Therapies
Our team shape and function will be reviewed to achieve our ambitions. We will strengthen our front door teams to maximise admission avoidance, working closely with community health and social care teams across the system to establish robust pathways. We will contribute to reduced inpatient length of stay and optimise outcomes and function through enhanced inpatient rehabilitation. We will increase screening and “prehab” for elective patients to improve clinical outcomes and more rapid, safe discharge. - Diagnostics
We will embed greater use of population health data to map predicted fluctuations in demand e.g. rise in autoimmune diseases or the use of genomic medicine.
Hospital to community
- Pharmacy
We will work with the wider system to create career pathways that enable staff to move flexibly across traditional boundaries between sectors, generating an agile workforce. - Therapies
We will continue to review of traditional ways of working moving more towards a non-medical model and review of pathways to gain financial benefits to the Trust and better pathways of care for our patients. - Diagnostics
We will deliver the integrated care system diagnostic strategy:
Create wider access to tests in the community to reduce health inequalities, enable prevention and self-management, and maximise screening and early intervention.
We will champion a community-first approach to ourdiagnostic pathways. We will develop one-stop pathways that enable elective diagnostic activity to be moved closer to patients (into primary care, CDCs, or other community health hubs). We will eventually compliment this with a wider range of services such as PET CT to reduce patient travel and delay particularly in the assessment and management of cancer.
Expand point of care testing options in patients’ homes and community services to support patients staying out of hospital. Patients will have greater access to tests in the community.
Analogue to digital
We will optimise our EPR and reporting to track capacity and demand across therapies and pharmacy. We will use AI and digital solutions to assist clinical decision making e.g. AI decision tools in pharmacy and antimicrobial stewardship.
- Pharmacy
We shall work with Higher Education institutions to develop a workforce to meet the growing demand in core clinical services that combines both traditional roles with alternative roles and advanced practice. This will consider greater digital enablement and use of AI, as well as the need for extended days or service across seven days a week. - Therapies
We will use Connected Care data to improve communication with community partners and use digital technologies to provide more information to patients on discharge. - Diagnostics
We will explore CT postmortem as a tool to increase access and acceptability for families whilst maximising the use of resources.
We will integrate point-of-care and rapid-response lab testing alongside community diagnostics. There will be a need to consider future developments such as genomics, which will be factored into estates planning given the evolving space and equipment required.
Ageing well
An ageing population is the most significant driver of increasing healthcare demand. By the time people are aged 65-74, 40% will have two or more long- term health conditions. Such conditions may be associated with more frequent hospital attendance or admission and the risk of further complications
or deconditioning. Long lengths of stay are often experienced due to the constraints on social care and out of hospital support delaying discharge.
The community and older people’s medicine directorate delivers a holistic service integrated with primary care, secondary care, hospices and community teams. The directorate supports people of all ages with complex or end of life needs. Our services include:
- Community services including community nursing, community matrons, intermediate care, community physiotherapy and occupational therapy, specialist nursing and care home matrons.
- Hospital at home multi-disciplinary team providing an urgent community response and ongoing acute care in people’s place of residence to prevent acute admission and support patients at home.
- Integrated frailty liaison teams at Frimley Park and Wexham Park hospitals are multi-disciplinary teams of doctors, in-reach GPs, nurses, physiotherapists and occupational therapists, providing a specialised service for patients living with frailty who
attend hospital. - Older people’s medicine inpatient services: Provided in both acute sites and two community inpatient units.
- Supportive and palliative care (SPC) provided across Frimley Park Hospital, Wexham Park Hospital, Heatherwood Hospital, and our Community inpatient beds. The SPC teams are composed of multi- professional team members with expertise in various aspects of palliative care and medicine.
We are proud to have a forward-thinking team who provide innovative services aligned to the NHS Long Term Plan across our acute hospitals and community services in the south of our integrated care system.
We have adopted an integrated and collaborative approach with system partners to provide seamless pathways for our patients and have extended our footprint into the Bracknell area with the opening of Heathlands intermediate care unit.
We are proud of the performance at our community inpatient units regarding length of stay and the number of patients returning to their normal place of residence.
We have a culture of strong leadership and governance and have integrated quality improvement initiatives ensuring our clinical teams attend the Trust’s continuous improvement training.
The multitude of partners across organisational boundaries represents a challenge to patient experience and continuity of care. Further opportunity exists to prevent care defaulting to hospital in our system.
- Our population is living longer but experiencing more frequent comorbidities; we want to support our patients with services that are accessible, seamless, and focused on prevention. We want our patients to live as independently as possible, for as long as possible.
- We want to continue to be a regional and national leader in ageing well, community services and end of life care.
- We want to engage in further research opportunities in order to further develop our services.
- Our services will be digitally enabled with a ‘home first’ ethos. We want patients living with frailty identified and supported with holistic assessments across all our hospital specialties as we know this improves outcomes and experience. We will continue to develop the virtual hospital model, working alongside other specialists to deliver acute care close to home as an alternative to acute hospital admission. At end of life, we want our patients and their families to experience compassionate, coordinated care supported in their place of their choice.
- When care needs increase, we want the service response to be predictive, coordinated and proactive, to avoid crises and repeated hospital attendances, with care and input digitally enabled and provided closer to, or at home. Where hospital admission is required, we want to provide frailty attuned care, with the avoidance of deconditioning and delirium and the stay to be for as short a time as possible.
Hospital to community
We will develop community hubs in order to coordinate multidisciplinary care closer to, and in the home. Such “hub versus spoke” services will include our hospital teams but also primary care and integrated neighbourhood teams.
We will further develop the principle of complexity hubs to provide multidisciplinary input for complex care and care planning that requires secondary care resource. This will aim to minimise the multiple assessments in different clinics that currently add little value outside of a more holistic and joined up clinical assessment. They will also facilitate anaesthetic assessment, surgical work-up and prehab where operative interventions are required.
We shall further develop the frailty SDEC models on each acute site to assess and treat whilst avoiding unnecessary hospital admission.
We shall expand our successful community inpatient model to improve outcomes and decrease length of stay in the acute sites.
We shall work with Deaneries, Universities and Higher Education institutions to provide the workforce and skills required to support increasingly complex patients in their own home as well as other care settings. There is a need to ‘grow our own’ workforce, and therefore we will explore apprenticeship opportunities.
Treatment to prevention
We will use our population health data to inform the planning of services, recognising the demographic variation and deprivation across our ICS, with the aim of reducing inequalities in access.
We will use the combination of our population health data, digital platforms, and the potential for AI to identify our high-risk patients and plan preventative interventions and/or wrap around support proactively within their communities.
We shall develop a positive brand for older people’s medicine, frailty and palliative care – it is a complex specialism impacting every service.
As well as those working with older people’s services, we must equip staff across specialities with the confidence to care for their patients with frailty and complex comorbidities.
Analogue to digital
We will use population health data, digital platforms, and the potential for AI to identify our high-risk patients to intervene early and provide proactive support out the acute setting.
We will expand the digital opportunities and the virtual hospital concept in patients’ own homes to enhance care continuity through oversight, monitoring, and support. This will allow us to prioritise face-to-face care where it adds the most value, for example when comprehensive assessments are required.
We will work with system partners to address digital exclusion for patients, as success will be reliant on digitally confident and empowered patients and carers. We will invest in and develop digital confidence and competence in our workforce.
Out of hospital care
The move to out-of-hospital care is a cornerstone of our clinical strategy. By investing in neighbourhood models, infrastructure, and workforce transformation, we will create a more sustainable and responsive healthcare system that meets the evolving needs of our population.
This shift not only aligns with national policy but also ensures that our integrated care system remains at the forefront of innovative, patient-centred care delivery.
Providing more care in the community will require a significant shift in workforce models. Some of our clinical and support staff currently employed in acute settings will transition into roles within primary and community services.
Our neighbourhood-based care will allow us to deliver health services closer to where people live, promoting accessibility, integration, and continuity of care.
Our integrated care system is committed to delivering more healthcare outside of traditional hospital settings. This shift is essential to achieve several strategic objectives:
- Rightsizing Frimley Park Hospital: The proposed new hospital for Frimley Park relies on reducing dependency on acute settings to ensure the facility is appropriately scaled.
- Responding to growing healthcare needs: Across our geography, we see an increasing demand for condition management that does not require secondary or tertiary care. However, too often, such care defaults into acute settings, leading to inefficiencies and added strain on hospital services.
- Alignment with national policy: Following the Darzi Review, national policy mandates that NHS systems move significant volumes of activity from hospital to community and neighbourhood settings. This presents both an opportunity and a necessity for transformation.
- We will foster healthier communities by emphasising prevention and early intervention. Building on the success of our virtual wards and connected care information, we will be able to provide better care outside our hospital to meet the needs of our local population.
- We will improve patient satisfaction through more personalised and accessible care.
- Together with our system partners, we will build on the good work we have done around setting up neighbourhood-based multidisciplinary teams across our system. Building and operationalising new health hubs, with a focus on high- need areas will improve our out-of- hospital care and enhance system efficiency by streamlining care pathways.
- We will roll out advanced digital solutions to connect services and empower residents. We will focus on the effective use of our resources and provide care closer to home by reducing the dependency on acute hospital services.
Hospital to community
Our neighbourhood-based care will allow us to deliver health services closer to where people live, promoting accessibility, integration, and continuity of care.
Multidisciplinary teams will work collaboratively across primary, community, and specialist services to deliver comprehensive care plans. Through our place- based health hubs we will provide diagnostics and outpatient care.
We will continue to integrate services to design care pathways that bring together the best of primary, community, and acute care. This holistic approach ensures that patients benefit from the right care at the right time, without unnecessary reliance on hospital services.
Realising this vision will require a significant shift in workforce models. Clinical and support staff currently employed in acute settings will transition into roles within primary and community services. New workforce roles will also be developed to support emerging care models. We will create roles tailored to integrated care models, such as care coordinators and community-based specialist practitioners.
Treatment to prevention
We will invest in health hubs and other community-based facilities to house the expanded range of services outside hospitals. Our place- based health hubs will provide preventative services.
We will provide upskilling and training opportunities to ensure staff are equipped for their new responsibilities.
Analogue to digital
We will expand and enhance our digital ecosystem to connect all levels of the care delivery system. This includes remote monitoring tools and digital platforms that facilitate seamless communication and
data sharing.
We will develop and implement a connected digital infrastructure to support integrated care. This includes shared care records, real-time communication tools, and AI-driven analytics for proactive
care management.
We will equip our patients with digital tools, such as apps and home monitoring devices, to enhance self-management and reduce unnecessary clinical visits.
We will ensure our facilities are designed with flexibility and sustainability in mind.
Long term conditions
Our strategy for managing the long-term conditions (LTC) reflects a commitment to transforming care delivery for a growing and diverse population in partnership with our integrated care system and adjacent systems.
Of our population living with a long-term condition, 24% have two long term conditions and 20% live with three or more long term conditions. People aged over 85 years are more likely to be living with a long-term condition including frailty.
People living with a long-term condition are more likely to use health and care services. They account for 50% of all GP appointments, 64% of all hospital outpatient appointments, 70% of all hospital bed days, and 70% of total health and social care spend.
Long-term condition support plays a role in creating a more sustainable health care system. Supporting people living with long-term conditions can lead to a better quality of life. However, it is important that those with long-term conditions feel supported to manage their overall health and wellbeing.
By focusing on prevention, innovation, and person-centred care with our system partners, we can alleviate the burden on NHS services while improving outcomes and quality of life for our residents.
Living with a long-term condition often takes a toll on mental health. Anxiety, depression, and social isolation are common among this population.
Patients with multiple long-term conditions are less likely to be in work than those with none, and those with a mental health condition are even less likely to be in work than those patients with long term conditions.
Over 50% of our integrated care system population now lives with at least one long-term condition (LTC). This figure reflects the increasing prevalence of chronic illnesses within our communities and highlights the urgency for tailored, sustainable care strategies.
Additionally, over 25,000 individuals are managing multiple LTCs, placing significant demands on NHS services. The growing complexity of these patients’ needs underscores the importance of evolving our care models to address these challenges effectively and efficiently.
To meet the diverse needs of residents with LTCs, we are concentrating on three primary areas:
- Cardiovascular disease (CVD): Improving early detection, prevention, and management to reduce the burden of cardiovascular complications.
- Diabetes: Enhancing self-management support, integrating care pathways, and reducing complications through proactive interventions.
- Respiratory conditions: Expanding access to evidence-based treatments, home-based care, and rehabilitation services to improve quality of life and reduce hospital admissions.
- Working with our system partners, and through partnerships with public health and local communities, we will have a strong focus on prevention. Our care pathways will reflect the diverse needs of our population. Our patients will have greater equity and accessibility of care across our integrated care system and region.
- We want to be known for improving the health and wellbeing for all individuals with long-term conditions.
- Our long-term condition management strategy will rely on collaborative partnerships across primary care, secondary care, community health services, and social care providers. We will expand the capacity and capability of community-based multidisciplinary teams.
- We will scale up our digital health solutions to improve access and streamline care delivery. We will work with partners and teams to reduce the demand on acute and urgent care services. We will work effectively, productively and efficiently through digital integration.
Hospital to community
We are committed to a neighbourhood model that delivers care in primary and community settings whenever possible. Acute hospital care will be reserved for cases where the seriousness of a condition warrants it. This shift reduces the burden on hospitals while ensuring patients receive timely and appropriate care.
By redesigning services, we aim to reduce the dependency of high-need residents on intensive NHS resources. Our multidisciplinary teams will deliver person-centred care plans, ensuring seamless coordination across health and social care settings.
We will enhance employment and wellbeing opportunities, supporting individuals with long-term conditions to engage in meaningful employment and community activities will foster a sense of purpose and improve mental wellbeing.
Instead of relying on traditional urgent models, we will provide more rapid response specialist care through advice and guidance pathways linked to Community Diagnostic Centres and targeted Tier 2 services (cardiology, ears nose and throat and musculoskeletal).
Complexity hubs linked to Community Diagnostic Centres will allow health better holistic care of overlapping long term conditions, such as multimorbidity in frailty and metabolic cardiovascular disease.
Treatment to prevention
Working with our system partners we will have a proactive focus on prevention and early intervention that will help reduce the onset and progression of long-term conditions.
Initiatives will include health education, regular screening programmes, and targeted lifestyle interventions.
We will deliver holistic person-centred compassionate, effective care: Treating the whole person, not just the condition, will improve overall outcomes. By focusing on physical, mental, and social health, we can help individuals achieve greater stability and independence.
We will embed psychological services within the long-term conditions care pathway, ensuring that individuals receive tailored mental health support as part of their overall care plan.
We will work with our system partners to enable the local population with LTC to age well and keep independent through proactive care, rehabilitation, reablement and though our senses services – hearing and sight.
Analogue to digital
We will harness digital innovations to improve productivity, responsiveness, and accessibility.
We will leverage remote monitoring devices, telehealth consultations, and integrated digital care records, which empower patients and clinicians alike.
Our people will be empowered through digital technologies.
What our strategy means
Our strategy will mean that our patients and local populations…
- Receive excellent, compassionate, seamless integrated care.
- Have more timely access to diagnostics and treatment.
- Are seen and treated more often in a community setting closer to home or in the comfort of their own home.
- Use digital and technological innovations to support their health and care.
- Will be living healthier, more independent and longer lives.
- Are empowered to self-care and take an active part in their health where appropriate.
- Will have access to timely, relevant and easy to access information about their care.
Our strategy will mean that our people…
- Are nurtured to be agile, adaptable and developed for the future.
- Feel valued, proud and respected in all that they do.
- Are supported to continuously develop themselves and their services.
- Feel treated equally and with fairness, celebrating difference.
- Deliver high quality services every day.
- Work in high quality, modern and sustainable facilities.
- Work productively, efficiently and effectively so that our money is spent well.
Our strategy will mean that our patients will be living healthier, more independent and longer lives